- Home
- Genetics: present and future
- Cloning and stem cells
Cloning and stem cells
What is cloning?
Cloning is a set of laboratory methods and techniques that allows us to reproduce any biological material as many times as we want, specifically cells, DNA, etc.
We could say that cloning is the same as photocopying, that is, to make as many identical copies of something as we need.
And, in our case, what do we want to clone or photocopy?
Very easily, what we want to clone are very special cells called stem cells.
What are stem cells?
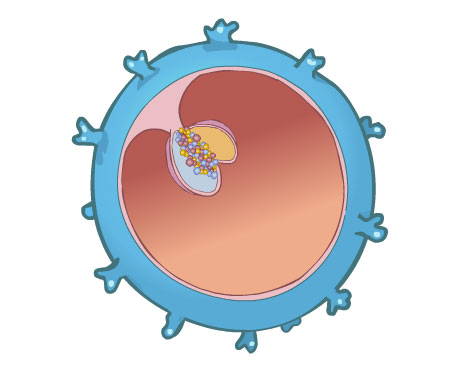
Stem cells are undifferentiated or unspecialized cells without a specific function because they have not yet changed into specific tissue cells. Stem cells are different to other body cells because during division they present the following characteristics:
- They produce new copies of themselves indefinitely.
- They produce new cells that under the right stimuli can develop into different tissues of which the human body is composed of.
- They can colonise and repair sick tissues or organs, replacing sick cells with healthy cells.
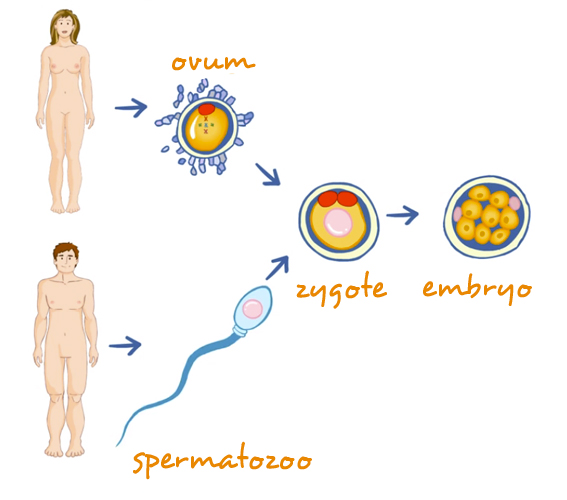
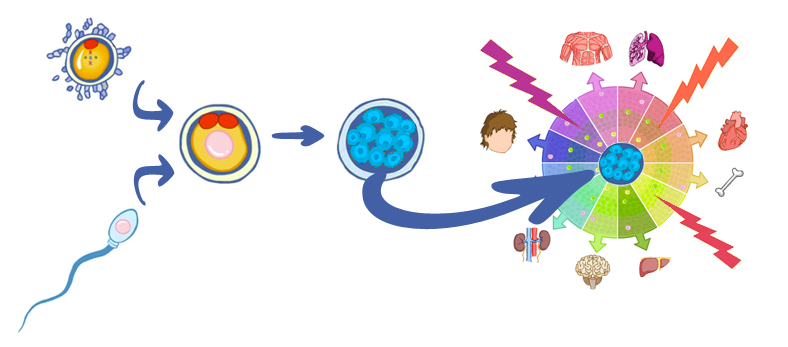
Stem cells are cells from which each of us developed after the ovum is fertilized by the spermatozoon. Stem cells are the cells that gave rise to all the tissues and organs that make up our body when they were subjected to specific stimuli. All our organs and tissues maintain a “small reserve” of these cells that allow for the maintenance and repair of tissues and organs.
Why is there so much interest in cloning stem cells?
There is so much interest because stem cells, aided by genetic engineering, are to become two fundamental pillars in medicine in the very near future.
Because when we achieve the appropriate combination of knowledge from genetics, medicine, physics, chemistry, molecular biology, cell and tissue engineering, biology, biochemistry, etc. from one or very few stem cells, we will be able to design and create cells and specific tissues to repair damaged organs or structures in our body and we will be able to produce therapeutic human proteins. This is known as regenerative medicine.

For example in Parkinson’s disease, it will be possible to replace damaged cells for new nerve cells and the affected individual will heal.
For instance, it will be possible to replace cardiac cells that have been damaged by infarctions or cardiac insufficiency with new and healthy cells and the affected individual will heal.
We will be able to repair medullary lesions caused by tumours or accidents. It will be possible for people suffering from diabetes to have insulin-producing cells transplanted into the pancreas and as a result and the affected individual will heal.
The same will occur with many other diseases such as cancer, cystic fibrosis and degenerative diseases like Alzheimer’s, etc.
Where do we stand right now?
We know that during their specialization or transformation, the cells in our body undergo specific cellular organ programming,
And that all the cells in our body have developed from one single cell, “the egg or ovum fertilized by a sperm cell”, which is why all of them are identical, meaning they poses the same exact instructions, but, depending on the organ they belong to, they will use only some part or other of the information. This is known as cell specialization.
In other words, all human cells possess 46 chromosomes engraved with all our kitchen recipes or “building blocks” (genes). However, these recipes are not manifested in all cells at the same time. Instead, some of the recipes are used on certain cells, and other recipes are used on other cells.
Due to this, the lung is different to the eye because the recipes pertaining to the lung contain information for the formation of cells specialized in respiration, and the recipes in the eye give place to the formation of an organ that allows us to see.
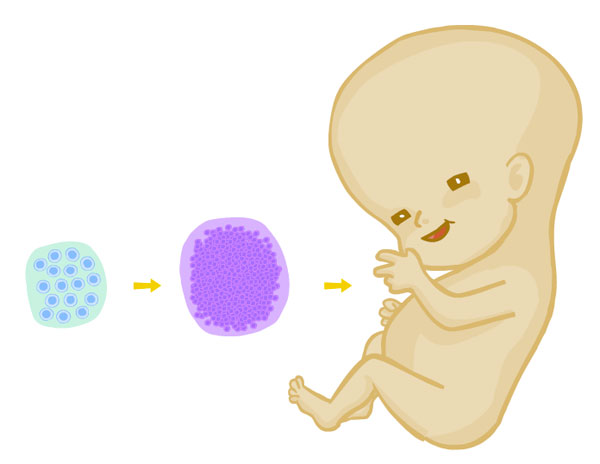
In other words, from an undifferentiated cell a complete individual has developed with millions of differentiated cells that make up different body structures. This means that during the development process the cells specialised.
So, from the moment of fertilization to the birth of an individual and throughout his/her life, cells undergo a process of differentiation or cell specialization under the commands of specific cellular programming for each species.
These cells in their early stages of embryonic development have the ability to produce a complete living being, meaning they are able to give origin to all the tissues of the new individual, including the extra-embryonic membranes that form the placenta. That is why they are called totipotential stemcells. Then, as gestation takes it course, they lose part of that potential because they become more and more specialized, and according to their transformation or differentiation possibilities they receive different names:
- Pluripotential stem cells are those capable of transforming themselves into all the tissues that compose a living being, except the extra-embryonic membranes (placenta).
- Multipotential stem cells are those that can be differentiated or that can be transformed into some tissues, but not all.
- Unipotential stem cells are those that can be transformed into just one type of cell tissue.
And, what does this all mean?
The answer is simple!
- THIS means that if we learn how to stimulate, programme and deprogramme these stem cells in a very near future we will be able to generate worldwide therapeutic tissues, new cells that will colonise and will repair damaged or sick tissues, replacement organs and new drugs and therapeutic proteins.
- THIS means that if we are successful in developing new methods of genetic engineering to be used in gene therapy, we will be able to correct genetic abnormalities of stem cells before they undergo differentiation into tissues or specific tissues, thus preventing disorders or malformations.
- Moreover, THIS means that if we are able to achieve this challenge with stem cells from the tissues of the actual individual, we will be able to repair and colonise all damaged organs or tissues with cells from the actual patient, thus resolving not only the important problem of immunological rejection to donor cells but also shortening long waiting lists for transplantation. Generation of stem cells will stop illegal organ trafficking in the black market.
Can you imagine if we could deprogramme with no side or collateral effects a cell that is already programmed and re-programme it again to our convenience? Wouldn’t it be great?
Are all cell the same or are there different types of cells?
There are three different types depending on the time they are obtained:
- Embryonic stem cells.
- Adult or somatic stem cells.
- Induced pluripotent stem cells, also known as iPS cells
How do these stem cells differ from each other?
- Their difference lies with the potential capacity (totipotential, pluripotential, unipotential) that each cell has to transform into different types of cells or tissues that compose our body.
- Their different capacity to self-renew (to produce new copies of themselves)
Embryonic stem cells and adult or somatic stem cells originate naturally. Induced pluripotent cells are artificial or laboratory-grown.
Let´s see:
Embryonic stem cells and adult or somatic stem cells occur naturally, in terms of their origin, that is, they are the same stem cells that receive different names depending on the evolution/maturation state they are in, may that be: in an embryonic stage, fetus, child, adult, cadaver. The cells are not altered or manipulated in a lab setting. In simple terms, they follow their natural course.
When these cells are part of the same embryo, they are called embryonic cells.
When stem cells are part of the tissues of fetuses, children, adults, umbilical cords, placentas and cadavers, they are called adult or somatic stem cells. Each tissue or organ in our adult body (postnatal), has a cell reservoir of these cells and these cells replace our sick or dead cells and repair damaged organs naturally, for example when a bone is broken it becomes fused again; when the skin or a muscle is injured, they heal and regenerate …… and this happends over and over again.
Induced pluripotent stem cells are manipulated (artificial) cells, as they were obtained at the laboratory by deprogramming adult stem cells.
And, what can we do in the mean time?
We must do research and learn to identify all the sings a cell yields to form a specific organ.
Where can we obtain stem cells to investigate and achieve our objectives?
It’s simple. They can be obtained from:
- Embryos
- Foetus
- Amniotic fluid
- Umbilical coord blood sampling
- Umbilical coord tissue
- Placental tissue
- Adult individuals
- iPS cells (Adult rerogrammed cells)
Embryos are the source of EMBRYONIC STEM CELLS. To obtain embryonic stem cells, we first need to produce embryos and allow them to grow for 5 to 7 days in the laboratory so that they start developing and transform into a blastocyst.
Once this has been achieved, THE EMBRYO IS DESTROYED, and cells inside of it known as internal cell mass are removed to be grown in the lab. Stem cells originate from these newly obtained cells.
And, how can embryos be produced?
It is not difficult. Embryos can be produced in the laboratory employing any of the following techniques:
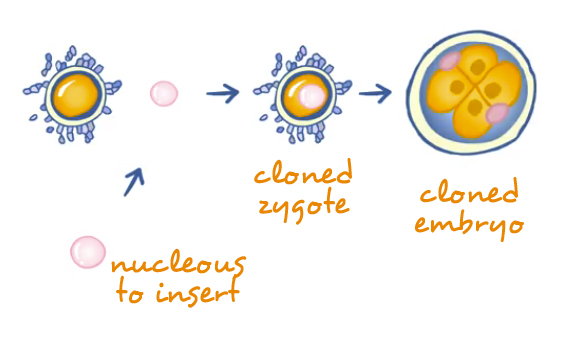
Once we get the embryo and depending on its final usage, we can choose between two types of cloning:
The use of all this technology poses several ethical and moral dilemmas.
For further information, please visit related links on this topic.
Foetal tissues or organs are obtained from miscarried babies (foetuses). These tissues or organs can provide TWO types of stem cells: germinal embryonic stem cells (with characteristics of embryonic stem cells) and adult or somatic stem cells.
- GERMINAL EMBRYONIC CELLS are obtained from embryos-foetuses aged between 5-10 weeks, from an anatomical structure known as gonadal crest. Under normal conditions these cells would give raise to the ova and the spermatozoa during the fertile life of the individual.
- ADULT OR SOMATIC STEM CELLS are those obtained from the remains of foetal tissues in foetuses of any age. Adult stem cells obtained from foetal tissues have less potentiality than embryonic stem cells for they are in a more advance stage of differentiation. However, the results obtained so far with these cells are encouraging.
Some experiments report that transplanting neuronal cells obtained from human foetuses has a therapeutic effect in patients suffering from Parkinson´s disease, with a noticeable reduction of the symptoms in treated patients. However, the procurement of foetal neuronal tissue or foetal tissues in general are very limited so there are several antiabortion groups that are totally against obtaining this type of cells in order to prevent many women from being induced to have an abortion of healthy foetuses just for the sake of obtaining and then selling these tissues in the illegal black market.
It has recently been shown that the amniotic fluid contains fetal mesenchymal stem cells, similar to embryonic stem cells. That is, pluripotent stem cells, which under appropriate stimuli, could become future repair cells of various body tissues.
At this moment in time, the potential in this research field is immense, as pointed out below:
- These cells are very similar to embryonic stem cells in terms of their potential for growth and differentiation; with the added advantage that once developed they do not create tumors.
- If necessary, if a sick fetus were to be detected during pregnancy, these cells could be extracted from the amniotic fluid, reprogrammed and be used during gestation to prevent the advance of the disease and if this is was not possible, they would already be prepared and ready for when the baby is born.
- In addition, these cells would present no immunological risk for the baby born from this pregnancy, as these cells come from the fetus’s own placenta and amniotic fluid.
- These cells could also be stored in cell banks, same as stem cells originating from the umbilical cord, constituting a reserve of immunologically compatible tissues for use by the world population.
- Nor would there be an issue from an ethical point of view, as their use does not involve the destruction of the embryo and there are studies showing that these cells can also be obtained from the placenta after delivery, besides the amniotic fluid.
Early experiments with these cells have already been conducted in mice.
Blood from the umbilical cord is a source of ADULT OR SOMATIC STEM CELLS.
The procurement of these cells does not pose any legal or ethical dilemma and good results are being obtained through their use.
Adult or somatic stem cells are obtained by puncturing the vein of the umbilical cord during the first 15 minutes following the birth of the baby.
Given the great therapeutic potential of these cells for the world population as well as for the donor and his or her family, we invite you to visit the related web pages by clicking on their links so that you can assess.
Cells from the umbilical cord are a source of ADULT OR SOMATIC STEM CELLS.
This tissue is made up by different types of cells that might have different potential uses, all of which are at an investigational phase.
Cells originating from placental tissue are a source of ADULT OR SOMATIC STEM CELL.
All these cells are at an investigational phase.
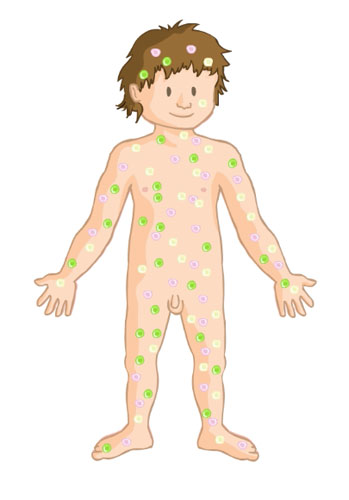
ADULT OR SOMATIC STEM CELLS can be obtained from the tissues and organs of adult individuals. We know that these undifferentiated stem cells are found as part of totally differentiated tissues and organs and that furthermore:
- They are present in many adult tissues (bone marrow, blood, cornea and retina, brain, skeletal muscle, gums, liver, skin epithelium, epithelium from the digestive system, pancreas and adipose tissue) and that new ones are constantly being discovered.
- They are responsible for the variability of tissues subjected to stress and constant regeneration, such as the skin, blood (bone marrow), intestinal mucosa, brain and adipose tissue, etc.
- They play a part in the regeneration of damaged tissues.
- They have more properties than initially thought, among these, plasticity, an ability to produce different types of tissues when they are isolated from the tissue which they form part of and are subjected to the right stimuli.
What are induced pluripotent cells?
Induced pluripotent stem cells (iPSC) are adult cells that have undergone genetic reprogramming to bring them back in time to earlier stages of development and convert them to a state similar to what they were in when they were embryonic stem cells, thus forcing them to express the same genes and the same factors that they expressed at that time.
What does it mean that they have been reprogrammed or dedifferentiated to a similar state to that what they were in when they were embryonic stem cells?
The answer is easy, let´s review and update our knowledge:
1) We know that at the time of fertilization when the egg and sperm unite, an egg is formed and it begins to divide until a complete individual is formed.
LET’S SEE HOW IT WORKS:
2) We know that cells arising from the first cell divisions that occur in the embryo have the potential to be converted into any body tissue. Then, gradually, as they start to differentiate into a particular tissue, they begin lose this property.
So, you will agree with me that THE CELL HAS SPECIALISED OR PROGRAMMED, correct?

Well, now, let´s do this inversely:
Let´s deprogram an ADULT cell that has become already specialized in a particular tissue, bringing it back in time to the EMBRYONIC STEM CELL stage in which it had the potential to become any tissue in the human body. Did you get it?

Well, there it is! This cell that we have deprorammed at will is what we call induced pluripotent cell (iPSC).
And, why are we interested in obtaining these cells?
Well, because we will be able to practice “ a la carte” reparative or regenerative medicine, that is “personalized and customized” medicine.
Imagine an individual who has suffered a heart attack. Well, from any of the individual´s adult cells (skin, muscle, etc.), and by employing the appropriate techniques, these cells can be retroceded in time to get them in the development stage where they were capable of producing cardiac cells. Once this goal is achieved, we will be able to get as many spare cells as needed to repair the said individual´s heart.
And, we will be able to do the same with all organs and tissues that make up the human body.
In other words, from the adult cells of a given individual, we will be able to deprogram and reprogram the individual’s own cells, thereby obtaining cells with the ability to become the specific tissues we are interested in or need to help cure such individual´s pathological condition.
And what advantages do these cells over other existing stem cells?
Because these cells are cells from the actual individual, there will be no immunological rejection. And most importantly, the origin of these cells does not bring up any ethical issues, as in order to obtain embryonic stem cell, the embryos are destroyed.
What is the clinical applicability of these cells at present?
There is no clinical applicability currently as they are still in investigational phase. Before these cells are used in patients, we must be completely sure that they meet all the necessary safety criteria, such as that they do not cause cancer or other diseases caused by changes or mutations that might have occurred during this process.
Who else can benefit from working or doing research with these cells?
Laboratories, as then they will be able to test the efficacy of the drugs directly on living cells from cell cultures.
Cell and molecular researchers, since all these strategies open up new doors for learning how to program, deprogram and reprogram cells to repair damaged body tissues of the body or introduce new features in the cells so that they express the characteristics that we might be interested in.
Since when do these cells exist?
iPSC induced in mice were first reported in 2006.
iPSC induced in humans were first reported in 2007.
If we were to ask ourselves the question “which stem cells from all the currently existing stem cells are the best for our purposes?” the answer at this moment in time would have to be NONE EXIST.
- At present there are more questions than answers. We must remember that development biology and tissue engineering are sciences that have just been started to be studied and much remains to be learned.
- No one knows with total certainty what the potential of stem cells will be when they are subjected to the appropriate stimuli.
- Advocating any specific cell type is full of private interests on the part of those who defend it regardless of the means or system used.
- These cells can be very useful in many research lines. Perhaps specific stem cells for specific research?
In view of the above, it would seem more prudent at this time to listen, assess and respect all opinions and to continue to perform research in all fields in search of the truth. And once we know where we are, then determine which direction to take. In doing this, we should not forget that the application of the available scientific techniques must always be correct from an ethical point of view. Making sure that this ethic code is complied with is the responsibility of all of US.
As it is already being done with stem cells from umbilical cord, all these cells may be stored in cell banks created for this end, constituting a worldwide reserve of immunologically compatible tissues for the general population.
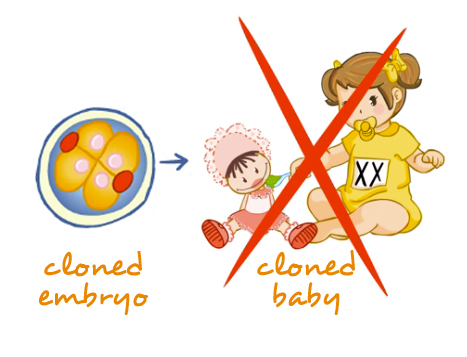
At present, the utilisation of embryos is the subject of debate among different religious, scientific, and political communities, for from a moral point of view “the use of embryos leads to its destruction” and the use of foetal tissues may induce many women to have abortions of healthy foetuses with the intention to procure this type of material.
What must remain clear is that during this learning period we must take great care when facing the enormous potential of these technologies. The “trial-error, trial-success, corrective measures” trilogy, can have unpredictable consequences for humanity, affecting us in many ways.
Summarizing …….
Related questions
Here you will find several links that might help you to understand the magnitud of the problem here presented.
Next topic: Genetics and cancer
Reviewed: 13th of September 2017